Dr Jackson Orem is on the front line of the change. He directs the Uganda Cancer Institute - the only dedicated cancer treatment facility in a country of 33 million people.
He's a busy man, but he makes time to see patients like Musa Settimba.
Settimba is in for a check-up. He has something called Gist, a type of gastrointestinal cancer that is often fatal, even in the West.
Orem has arranged for Settimba to get a very effective and costly new cancer drug free of charge, courtesy of the manufacturer. There's paperwork involved, and drugs for only a few cancers are available this way. It's a godsend for Settimba, who has been doing very well.
"You are getting one of the best treatments for this disease," a smiling Orem tells his patient.
Unfortunately, Settimba is the rare exception.
The survival rate for patients who make it to the Uganda Cancer Institute is astonishingly low. It treats about 22,000 patients a year, and of those, 20,000 die within a year.
Orem says most Ugandans don't have a real concept of cancer as a set of diseases that can be diagnosed and treated. In some tribal languages, there is no word for it. "They don't have early diagnosis. They don't actually even know that they have cancer," he says.
And most don't see the value of seeking care. "Once you are diagnosed with cancer, they think that it's already a death sentence."
They're partly right. Most people don't see a doctor until the very last stages of cancer. At that point, no hospital anywhere could do much for them.
Orem studied oncology in the US and returned to Uganda to head the government-owned cancer institute in 2004. For several years, he was the only oncologist in the country.
Orem doesn't complain about the hard work, but some things make him cringe. One of them is a comment he's heard expressed by people from developed countries - that cancer doesn't hit poor people.
"People think that malaria kills [and] other diseases are killing people from a low socio-economic status. But cancer is the same," he says. "The truth of the matter is that cancer is a disease of the African person just like any other person elsewhere in the world."
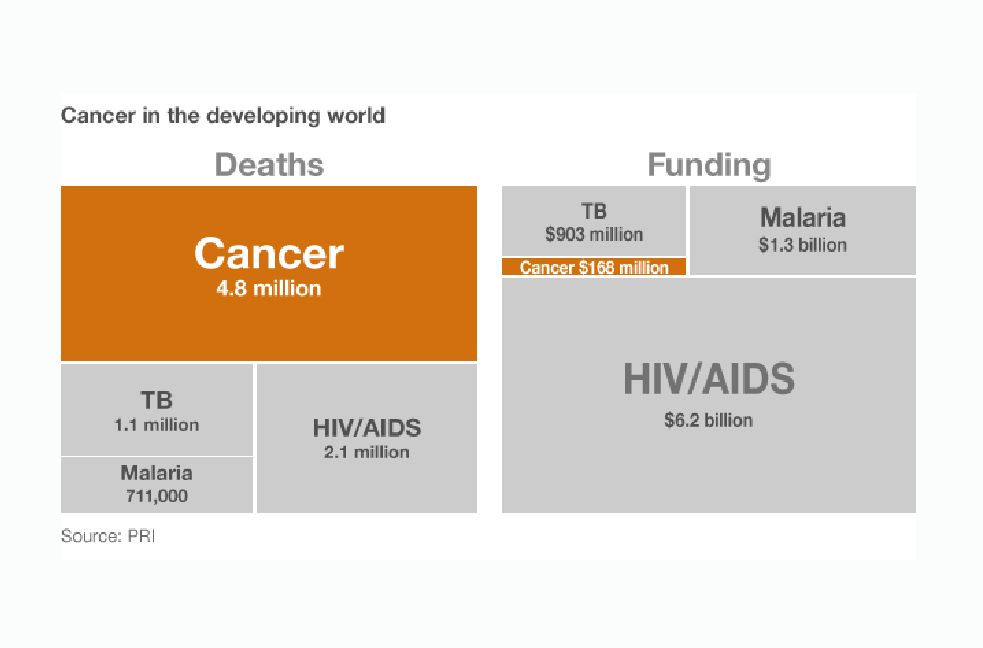
The misconception affects funding. "When you ask for funding for cancer, nobody is going to give [it to] you," Orem says. "But if you ask for funding for these other diseases, they say, 'All right, your priority is correct, we are going to give you some funds.'"
There is also a perception that cancer is too expensive to treat, and treatment is too hi-tech to be done in poor countries. Orem says that's not necessarily true - surgery and chemotherapy, for example, don't require million-dollar machines.
The result is that the amount of money available for cancer care in the developing world is only a fraction of the sums spent on HIV, TB and malaria.
"I think donors have been asleep," says Richard Horton, editor of the medical journal The Lancet. "It's an appalling example of neglect."
He blames donors who regard cancers caused by tobacco or obesity as the patient's fault, and not worthy of aid. At the same time, he acknowledges that HIV, TB and malaria have created an overwhelming burden.
"It's been hard to see anything through that fog of death," he says.
But as the HIV, TB and malaria numbers come down, things may change. "The clearing of the mist as a result of those successes has left [the cancer epidemic] in view," Horton says.
Last year, the UN urged that more be done to detect and treat cancer in the developing world. George and Laura Bush recently toured Africa to bring attention to breast and cervical cancer.
Orem, meanwhile, takes heart from changes in Uganda, where the government is putting up a modern 200-bed cancer hospital on a hill above the dilapidated one-storey tin-roofed buildings of the cancer institute.
He also has the help, now, of five Ugandan cancer specialists trained at the Fred Hutchinson Cancer Research Center in Seattle.
"People are much more receptive to our messages than before," he says. "It looks like we are beginning to make an inroad."
In Haiti, the poorest country in the Western Hemisphere, one NGO has found a different way to make an inroad in the treatment of cancer - through primary care.
Zanmi Lasante, together with Boston-based Partners in Health, focuses on breast and cervical cancers - the most common cancers among Haitian women - at a clinic in the little town of Cange. It has treatment rooms, chemotherapy and an operating theatre.
Dr Ruth Damuse says the biggest problem with breast cancer is that, just as in Uganda, women come in late, long after they've noticed the initial lump.
About half the women with breast cancer die, she estimates, and many sufferers don't come in at all. The clinic does what it can, and where it can't do much, it offers palliative care.
Earlier this year, on International Women's Day, Damuse went to a rally to preach early diagnosis. She took the podium and asked the crowd a question: "Which cancer most affects women?"
The crowd murmured. No-one knew.
"We're going to talk about breast cancer," she continued.
She showed pictures of breast cancer patients with tumours breaking out of their chests. She told the women how to check themselves for suspicious lumps and explained how treatment makes a difference.
The women near me said it was all new to them.
Treatment is also a challenge. There are no oncologists at the clinic, so the staff make a weekly phone call to the Dana Farber Cancer Institute in Boston. Before the call, they send patients' medical histories, lab results and what X-rays are available to Larry Shulman, head of the institute.
He reviews the records, then gets on the phone. In Haiti, a primary care physician, oncology nurse and several others gather around a speakerphone in a simple stucco house near the hospital.
During one recent call, seven patients were up for discussion. One woman had had a breast removed last autumn, but the cancer returned. Shulman suggested a different kind of chemotherapy.
Another young woman had had a breast lump removed. In developed countries, women who get lumpectomies generally get weeks of daily radiation treatments as well. But the Haitian clinic doesn't have any way to administer radiation. So Shulman suggested a full breast removal.
"She needs to go back and have a mastectomy," Shulman said over the phone. "Then she needs five years of tamoxifen."
Tamoxifen pills cost just pennies a day, affordable even in Haiti.
Cancer surgery, chemotherapy and after-care can be costly, however. Partners in Health and Zanmi Lasante provide this free of charge and rely on donors to cover costs.
Sara Stulac, the head of Partners in Health's cancer programme, admits that her team is taking on a big challenge.
"I think some people would say we shouldn't [tackle cancer], but the fact is people are suffering and dying," she says.
"We can't save all of them, and we can't save the same group of patients with the same group of diagnoses that we can in the US. But there is so much suffering that we can avoid, and there are so many cancers that we can treat."
Stulac points to another disease as evidence.
People used to say that AIDS drugs were too costly and too difficult to deliver in developing countries, yet millions of people with HIV in places such as Uganda and Haiti are now being saved. Stulac says there's no reason that can't happen with cancer.
Explore this interactive map to learn about cancers that disproportionately affect poorer countries.
This series of reports is by PRI's The World with support from the Pulitzer Center on Crisis Reporting.