Prodavinci analyzed the location of sentinel centers, 46 public health centers designated by the Venezuelan government to treat COVID-19 patients, and found important inequalities in their distribution. The distance between a COVID-19 patient and the health center is associated with mortality: people further away from treatment have a higher risk of dying. And yet, half of the Venezuelan population has to drive between six and 187 miles to reach a sentinel center. Rural populations have less access than people living in cities. The government’s center distribution does not respond to population density or health infrastructure.
In some cases, cities with large populations have no centers while small towns have one. In others, primary health care facilities are designated to treat millions of people, instead of nearby public hospitals with specialized equipment.
The resulting health coverage is uneven. Because of proximity, 26% of the country’s population would, potentially, seek COVID-19 treatment in three centers out of the 46 designated by health authorities in March 2020.
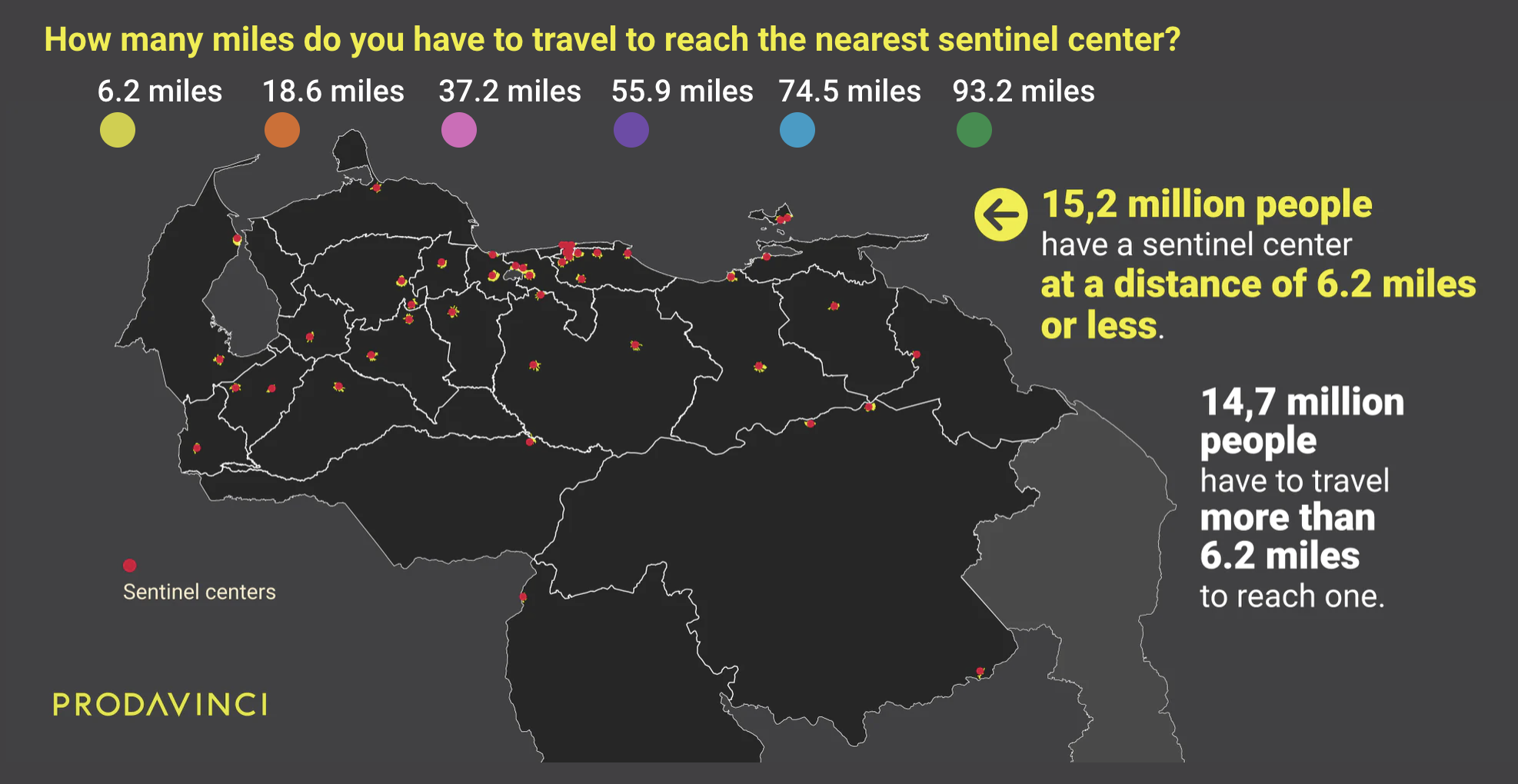
Distance between a patient and a treatment center matters. For COVID-19 patients in Lombardy, northern Italy, at the peak of transmission, mortality for men over 55 years old was 30 to 50 percent lower in municipalities with intensive care units (ICU), according to an analysis of death registry data by two economists for the Centre for Economic Policy Research (CEPR). Municipalities with ICUs farther than 6.2 miles (10 kilometers) away experienced 6 more deaths per day per 100,000 inhabitants compared to municipalities with an ICU in town – almost twice as much. For people living far away, ambulance congestion worsened access to medical attention.
“Sentinel centers” are building blocks of Venezuela’s response to the pandemic. “These 46 hospitals throughout the country [...] will head and enforce medical attention for coronavirus,” President Nicolás Maduro said on March 12, a day before the first detected COVID-19 case in Venezuela was revealed. Maduro’s government reported to the United Nations that sanitary investments, resources and equipment donations have been focused on these 46 sentinel centers. Even as local authorities have designated new sentinel centers since June, the official Health Ministry list has not been updated. The first sentinel center national map designated in March provides fundamental insights into the government’s epidemiological strategy to mitigate COVID-19’s impact in the country.
Using geographic information systems (GIS) and remote sensing data, Prodavinci analyzed road distances between 11,432 populations and 80 larger cities (with over 50,000 inhabitants), and all COVID-19 treatment centers. We located the nearest center for each population and measured travel distance. In doing so, we considered 267,484 highways, streets and avenues in Venezuela. This analysis focused on the geographic location of each center, not on their treatment capacity.
The distance between
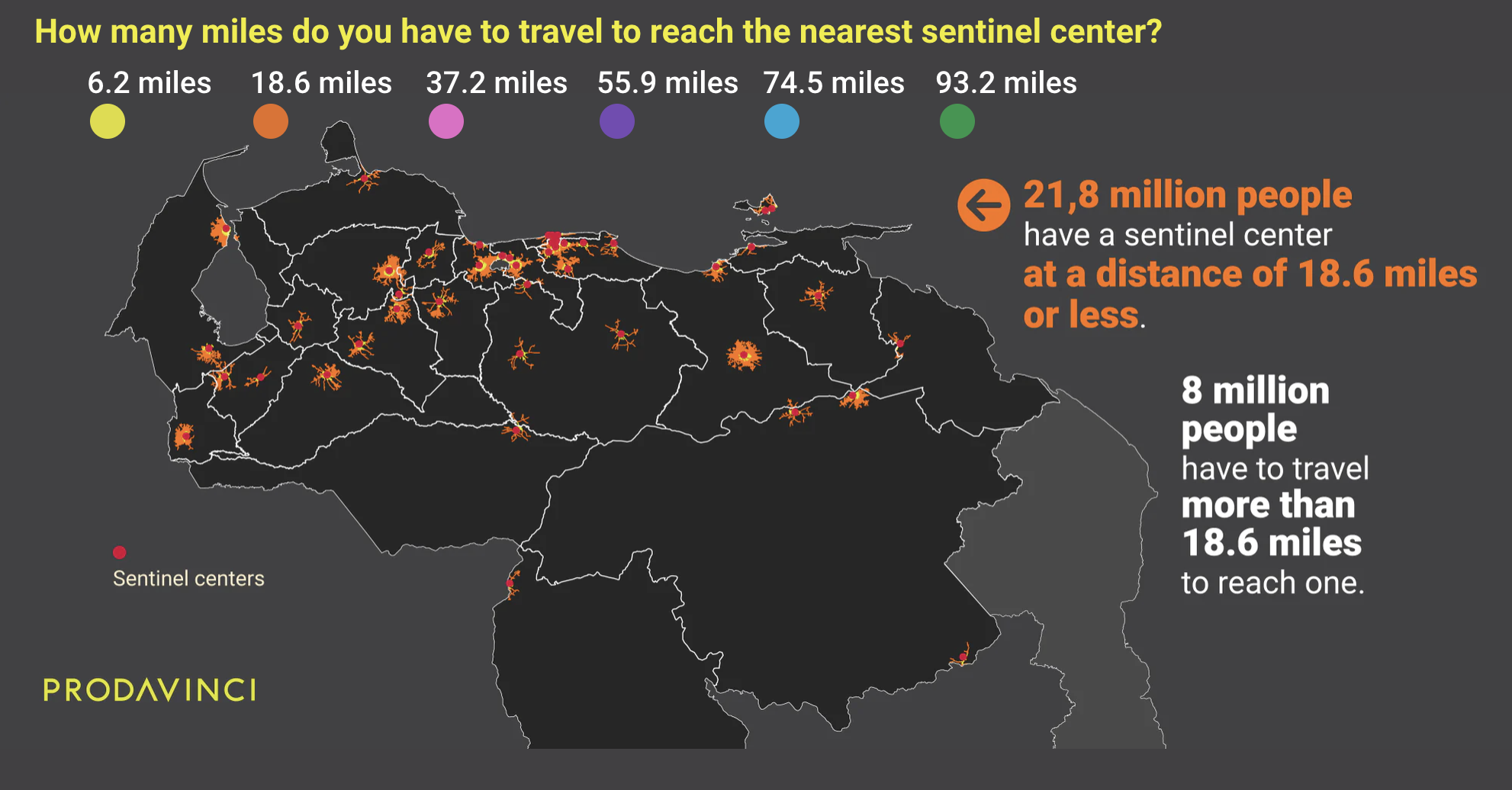
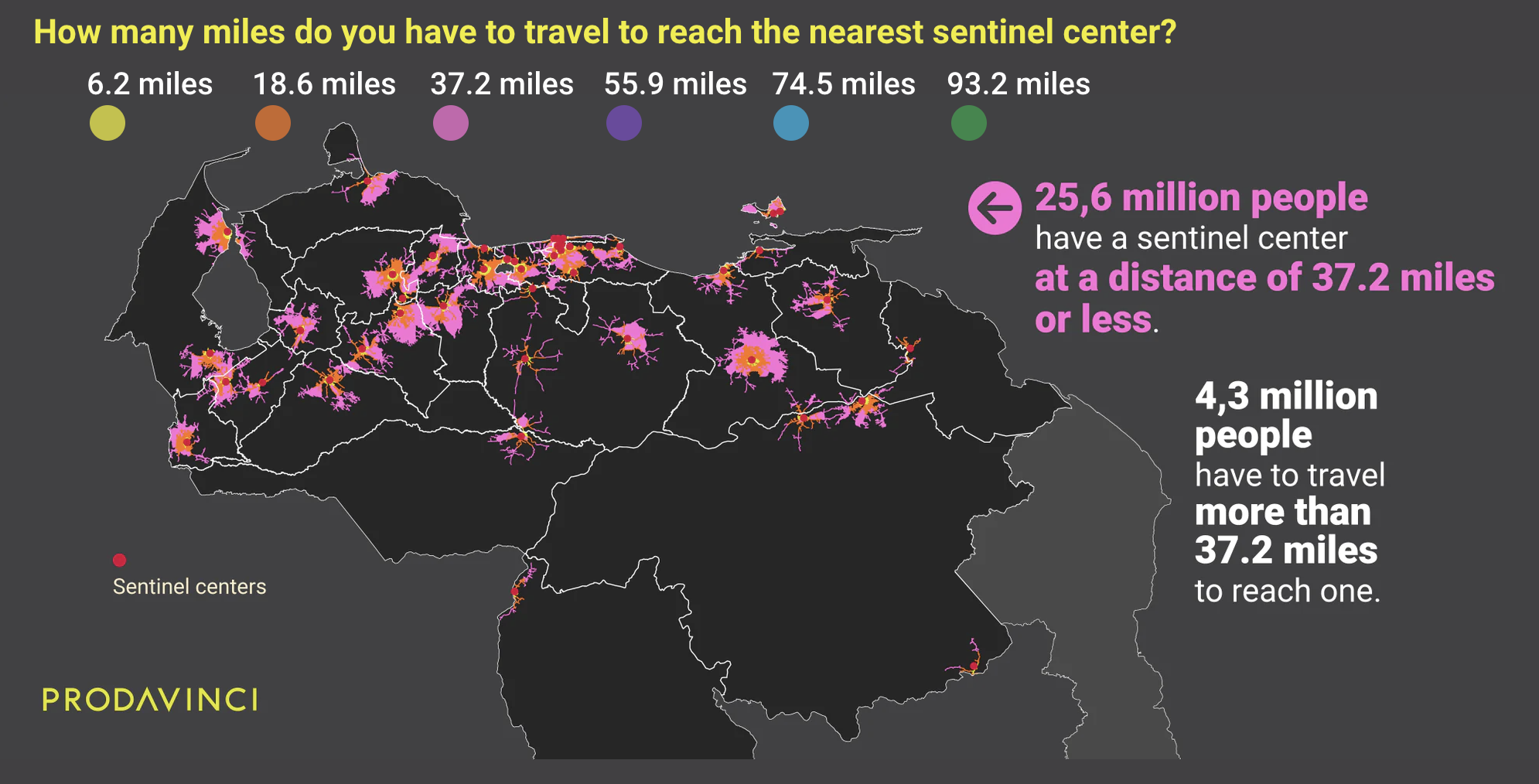
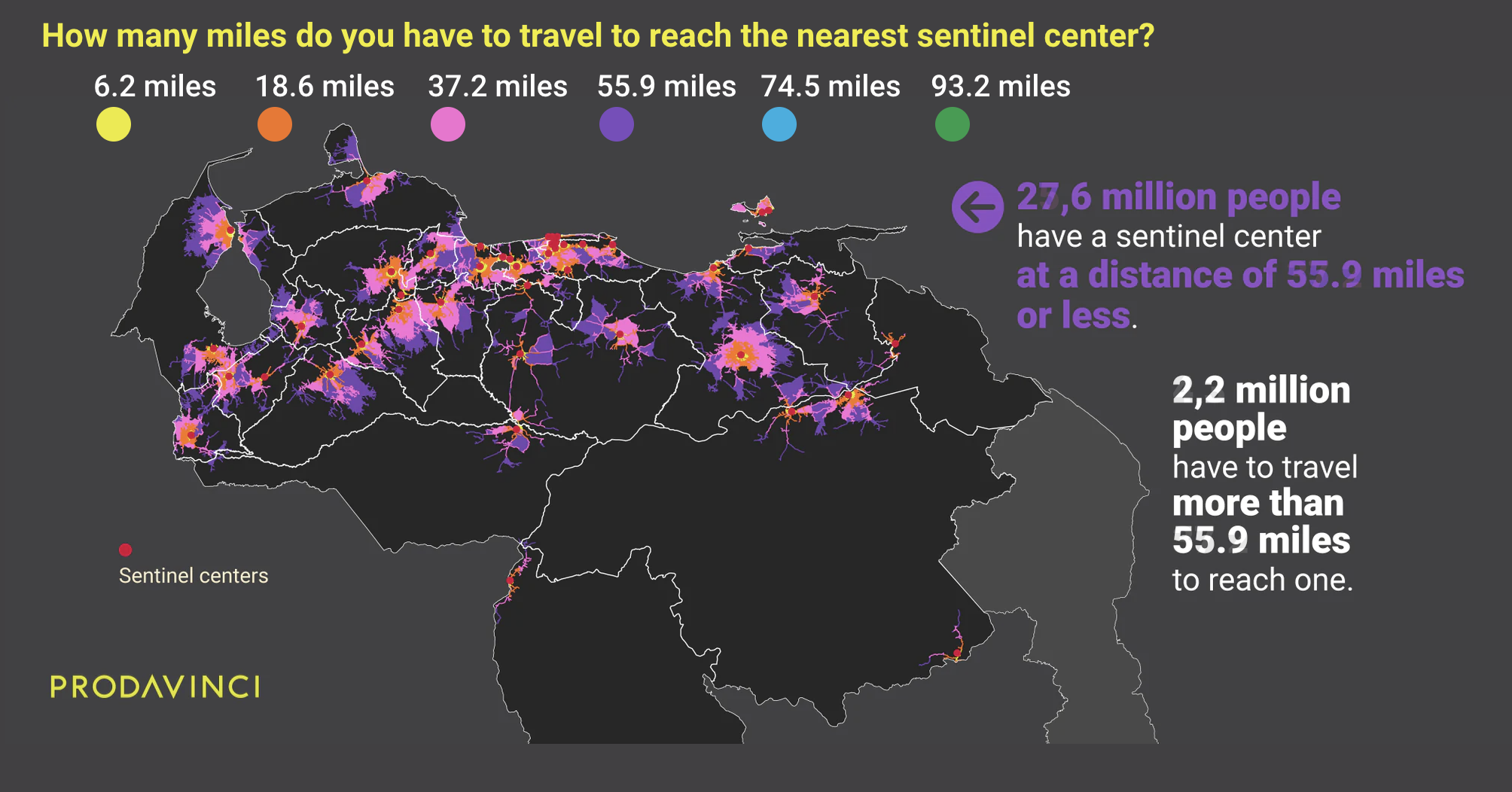
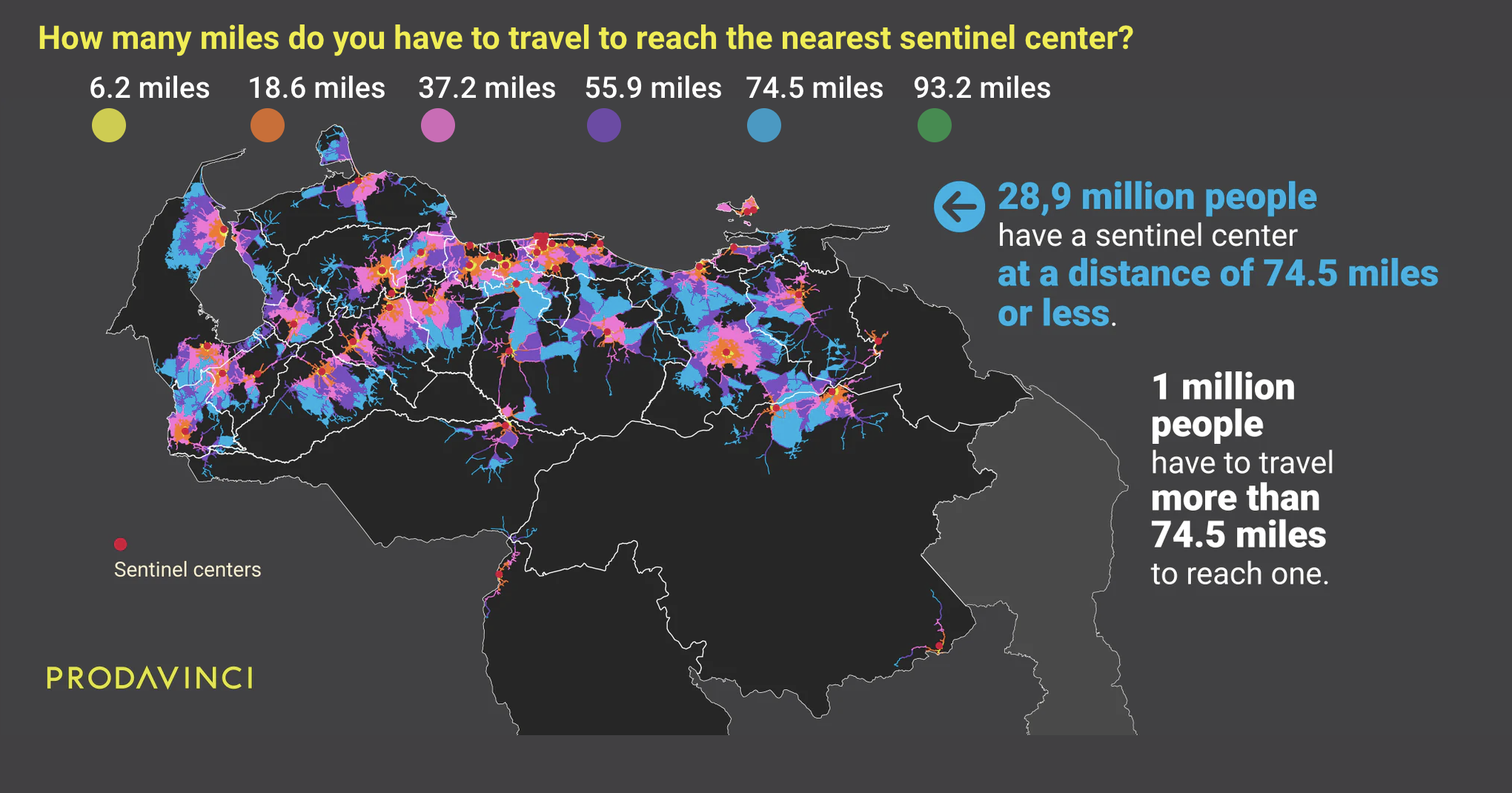
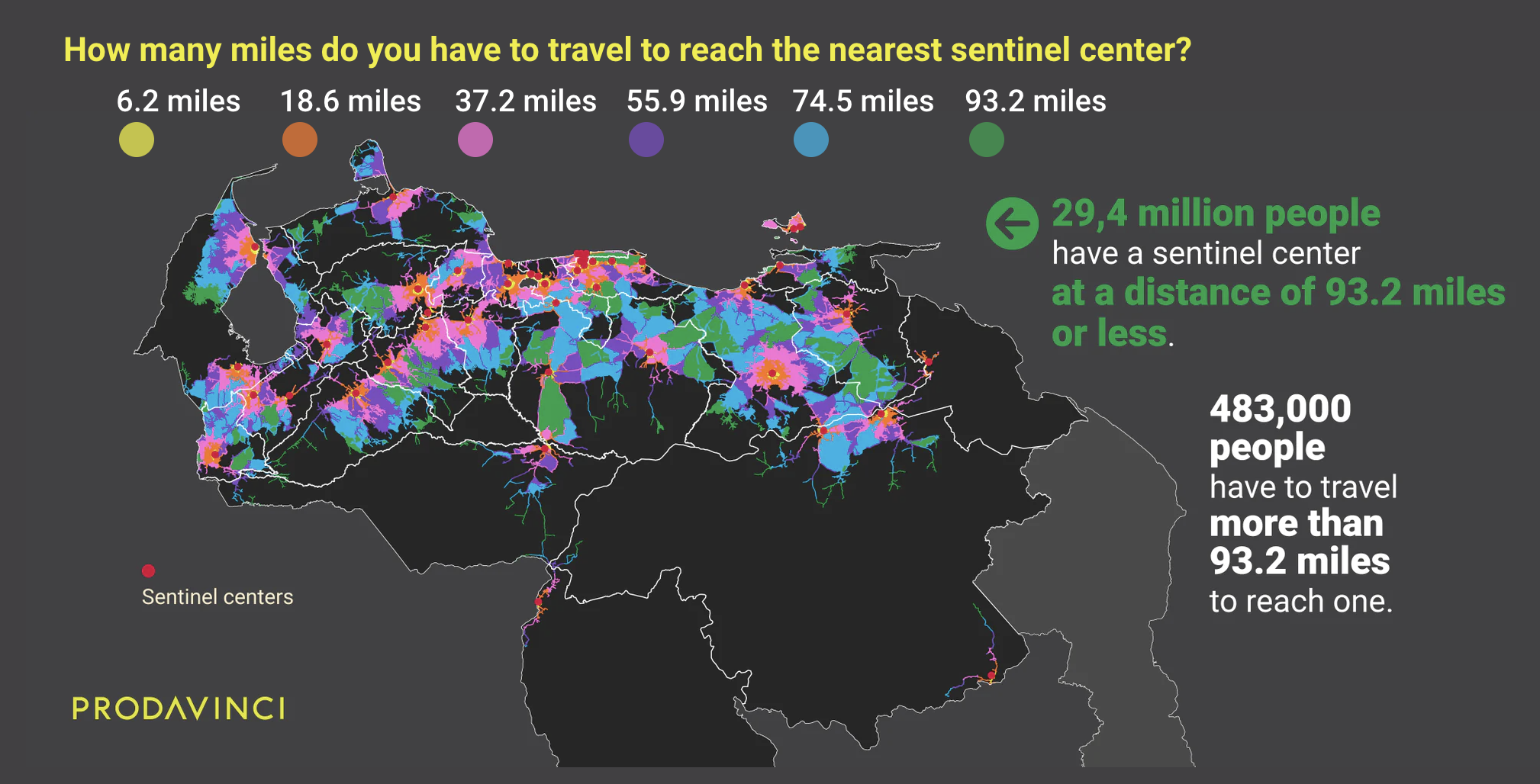
On average, Venezuelans have to travel 17 miles to reach the nearest COVID-19 treatment center. This map summarizes population distribution and their driving distances to reach the nearest public treatment center.
Sentinel centers and the Venezuelan population
Close to 70% of the Venezuelan population lives in cities with over 50,000 inhabitants. Most sentinel centers are located in urban areas but their distribution does not respond to the population density.
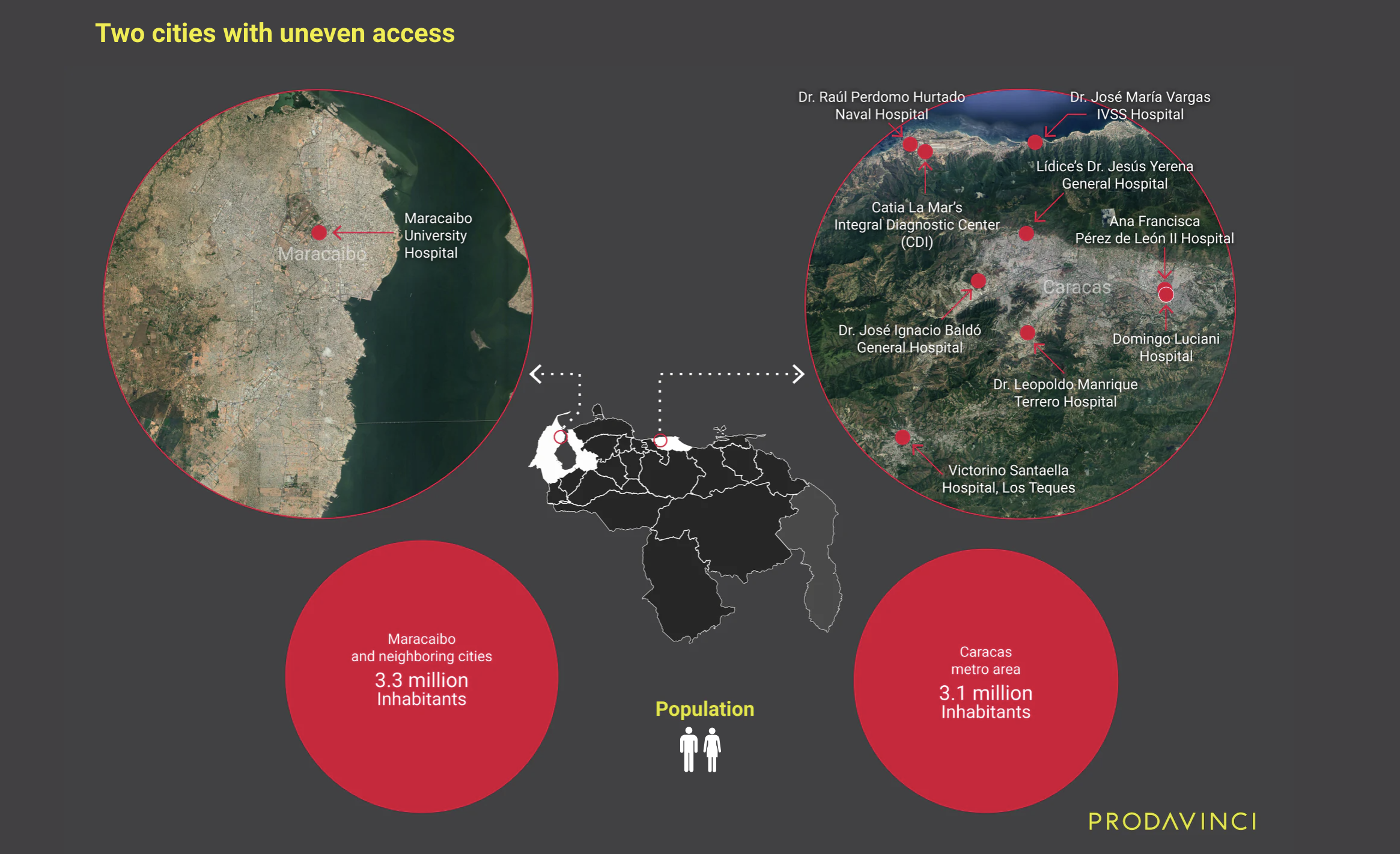
Zulia, the most populous state in Venezuela, has 4 million inhabitants and, in March 2020, the government designated only two COVID-19 treatment centers. In the capital region, Miranda state, the second most populous with 3 million people, had six centers.
Maracaibo, Zulia’s capital city and the second most populous city in the country, had only one COVID-19 treatment center. Maracaibo's University Hospital was the nearest center for over 3.3 million people, the largest served population by any single center. Seven cities with over 50,000 people depended on this hospital for COVID-19 treatment. The second nearest center was Dr. Pedro Emilio Carrillo University Hospital in Trujillo state, 140 miles away.
On June 8, Zulia’s governor, Omar Prieto, announced Chiquinquirá Hospital as the second sentinel center in Maracaibo and the third in the state. Ten days later, on June 18, the governor, and Marisel Bermúdez, vice minister of health, said Adolfo Pons Hospital would be the third center in Maracaibo, fourth for Zulia. But these new centers do not appear on official lists or communications. Patients with COVID-19 symptoms in Zulia don’t have access to an updated list of public treatment centers in their state.
In contrast with Maracaibo, Caracas, the country’s capital and the most populous city in the country with over 3 million inhabitants, had five sentinel centers in its metro area. Two in Sucre municipality and three in Libertador. But in an 18.6-mile radius Caracas has four additional centers: one in Miranda and three additional centers in La Guaira state. In total, the city’s population has nine available treatment centers within an 18.6-mile driving distance.
The following infographic compares Caracas and Maracaibo’s sentinel center distribution.
Center distribution does not correspond with available health infrastructure either. Zulia has 35 public hospitals but only two were designated as COVID-19 treatment centers. Miranda has 19 public hospitals, almost half as Zulia, and the government habilitated six of them.
Distribution does not correspond with health infrastructure, not only because of the number of hospitals, but because of their built capacity.
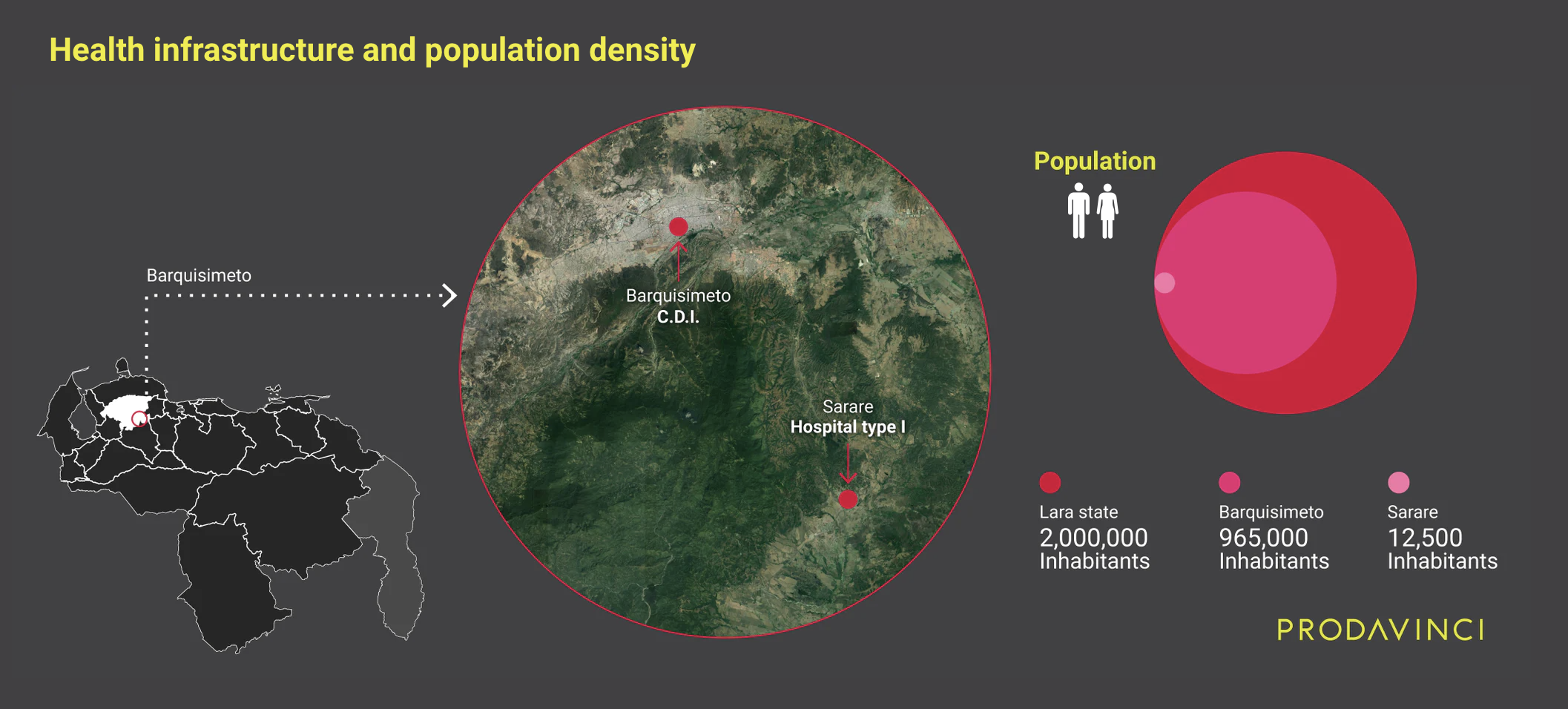
Lara state has less than 2 million inhabitants and the government designated two sentinel centers: a CDI, a primary health care facility, in the state capital of Barquisimeto, a city with almost 1 million people, and a Hospital type I in Sarare, a town of 12,500 people. The CDI has an approximate area, measured using satellite imagery, of 700 square meters. It is the closest public COVID-19 treatment center for 2 million people, including Barquisimeto, nearby rural populations and other small cities. In contrast, the Dr. Armando Velásquez Mago General Hospital in Sarare has an approximate area of 2,000 square metres and it is the nearest center for 30,000 people.
Sentinel Centers and the cities
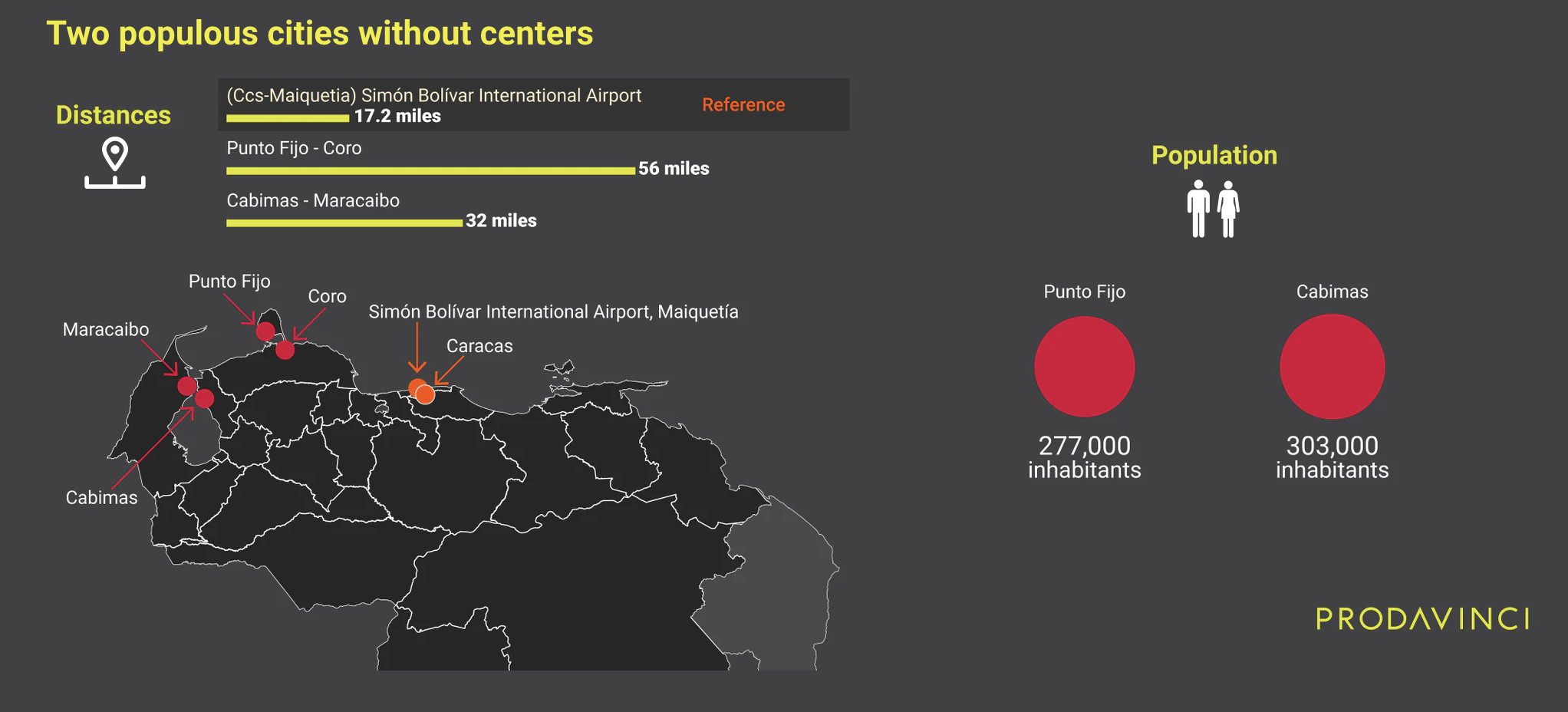
Out of the 20 most populous cities in Venezuela*, two do not have COVID-19 treatment centers: Cabimas, in Zulia state, with over 303,000 inhabitants, and peninsular Punto Fijo, in Falcón state, with over 277,000 people. The nearest treatment center for Cabimas is Maracaibo University Hospital, which is over 32 miles away. For Punto Fijo it is Dr. Alfredo Van Grieken University Hospital in Coro at a 56-mile driving distance.
For 8% of Venezuela's urban population, 1.6 million people, the nearest COVID-19 treatment center is more than 43 miles away.
Sentinel centers and rural areas
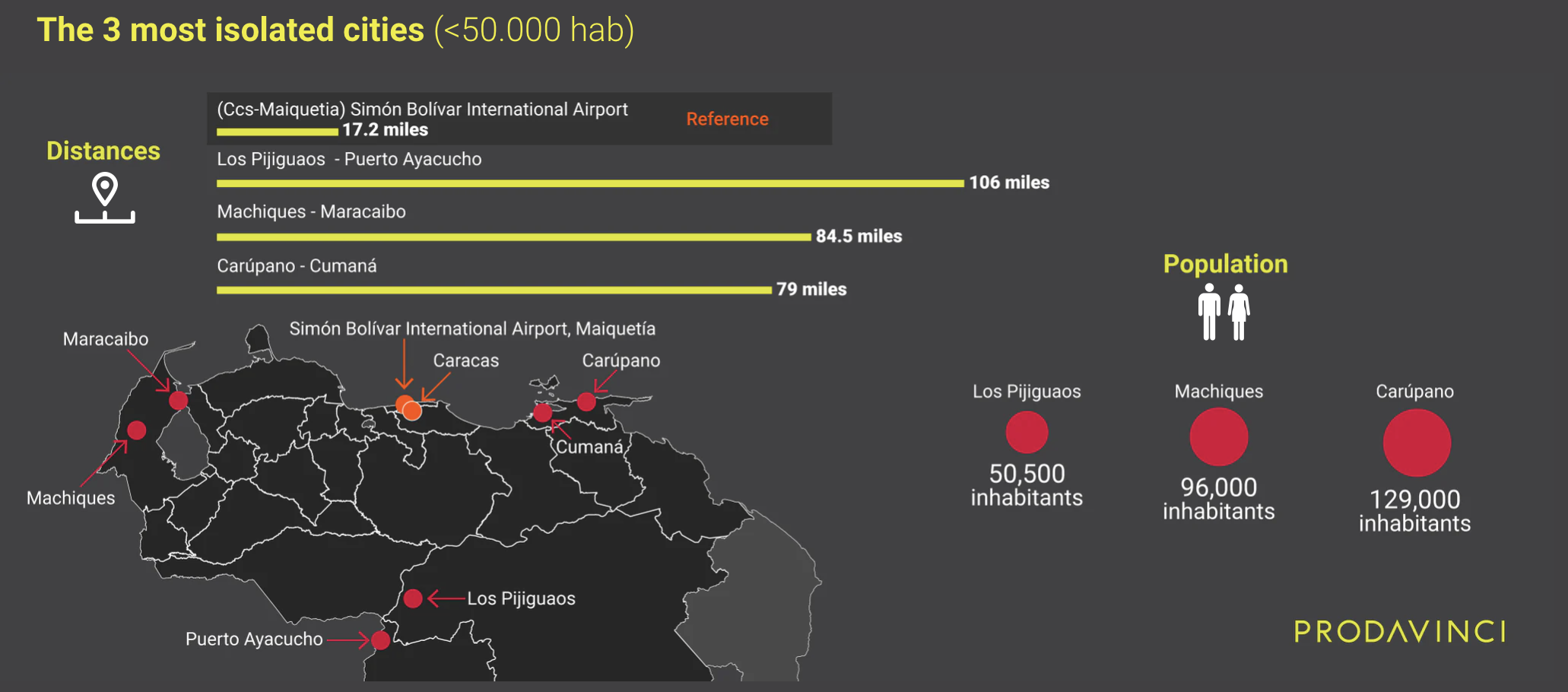
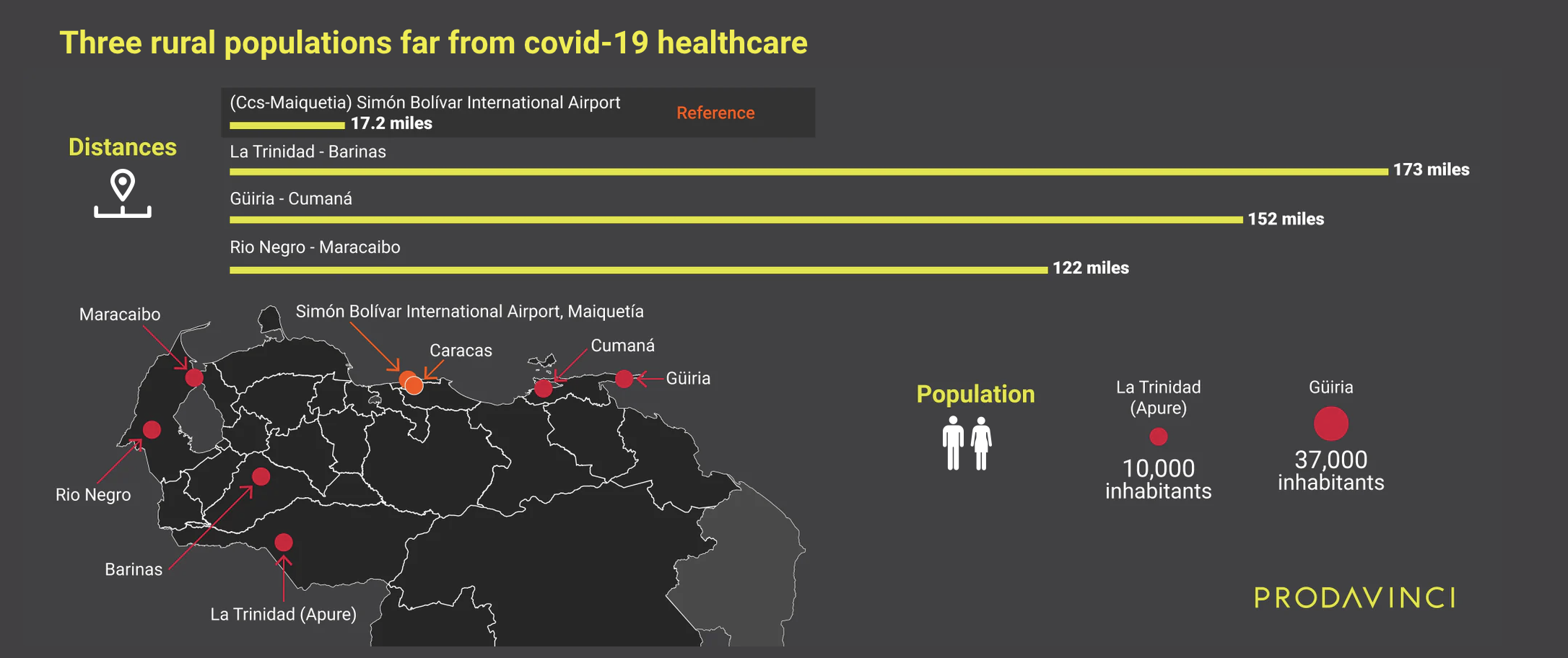
For rural populations, access to COVID-19 treatment centers is worse. Distances are larger. Any person with symptoms within the 10,000 population of La Trinidad, in Apure, has to travel 173 miles to reach Luis Razetti Hospital in Barinas; the nearest sentinel center. In Güiria, a fishing town in the southeastern tip of the Paria Peninsula that borders Trinidad and Tobago, any of its 37,000 inhabitants has to move 152 miles to reach the only center in the state. And in Río Negro, Zulia, people have to travel 122 miles to reach the nearest COVID-19 treatment center.
Out of the top 20 farthest counties (called “parroquias” in Venezuela) from a sentinel center, 11 are located in Sucre state. It is the state with the most counties without nearby public COVID-19 medical attention, followed by Apure and Falcón states.
Sucre state has little over a million people. 565,000 of them live in Cumaná, the capital city with the only sentinel center in the state, Antonio Patricio de Alcalá University Hospital. Araya, the most important town in western Araya Peninsula, a strip of land with 40,000 inhabitants, is 118 miles away from the hospital. In eastern Paria Peninsula, the distances are longer. People In Puerto Hierro, a border town with Trinidad and Tobago, have to move 163 miles to reach the nearest center. Paria has 328,000 inhabitants.
Only three out of 46 sentinel centers are located in rural areas: Higuerote’s General Hospital, Sarare’s General Hospital and Santa Elena de Uairén’s Rosario Vera Zurita Hospital, in the southern border with Brazil.
Unequal coverage and mortality
The government’s designation of 46 COVID-19 treatment centers does not follow population density or health infrastructure.
The geographic placement of these hospitals and CDIs leads to highly unequal access to COVID-19 treatment. Urban areas have few centers, like in Barquisimeto and Maracaibo. But rural areas, like Paria Peninsula in Sucre and Apure’s Llanos, have none. People have to travel long distances to reach a treatment center. This means few centers serve large populations, including nearby smaller cities and farway rural communities.
Seven sentinel centers would bear the burden of assisting 40% of the country’s population.
Maracaibo University Hospital was the nearest sentinel center for at least 3.3 million people. Dr. Enrique Tejera Hospital City, in Valencia, was the nearest for 2 million people. And Barquisimeto’s CDI was the nearest for an additional 2 million inhabitants.
The populations living in these three cities—Maracaibo, Valencia, and Barquisimeto—have a nearby public treatment center. But the national average is different.
Venezuelan authorities designated 46 sentinel centers days before the first detected COVID-19 case was revealed, on Friday March 13, 2020. On Monday, March 16, with 33 confirmed cases, national quarantine restrictions were announced. Cases were sporadic but transmission was growing. New outbreaks appeared. Two months later, on May 22, the country had 1,010 detected cases. There was community transmission. The government relaxed restrictions on June 1 with 1,663 cases, but reinstated them three weeks later as cases rose to 4,048.
When COVID-19 transmissions speed up, so does demand for professional medical services. One of the worst case scenarios in a pandemic is when demand for hospital resources outpaces capacity. When there aren’t enough resources to treat all severe patients, mortality rises.
In this scenario distances become important.
If a person in rural San José de Perijá, Zulia, has COVID-19 symptoms, they have to drive more than 88 miles to reach Maracaibo’s hospital. But this treatment center is also the nearest for Cabimas, Ciudad Ojeda, La Concepción, Machiques, San Rafael del Moján, Santa Rita and Villa del Rosario, seven additional cities with over 50,000 inhabitants each.
Patients far away from health centers also tend to delay travelling to the hospital. They wait for more severe symptoms to appear because moving implies resources and risk. But hospitals admit patients by order of arrival and have limited capacity.
Any patient living in rural Paria, in Sucre, has to travel between 80 and 167 miles to reach COVID-19 treatment. But once there, they still compete for space in the only treatment center in the state. That hospital is already assisting half a million people from Cumaná, plus 40,000 of Araya’s inhabitants and people from other states.
Even as rural populations travel long distances to reach treatment centers, when they arrive, these hospitals are already assisting their urban populations and people from nearby smaller cities. COVID-19 patients with severe symptoms living in the cities could also have trouble accessing medical attention for the same reason.
When the system is overwhelmed, distance makes a difference “because choices have to be made regarding who should be saved,” Gabriele Ciminelli, co-author of the Lombardy death registry data analysis, said to Prodavinci. Ciminelli is an assistant professor of finance and economics at Asia School of Business and ex-researcher at the International Monetary Fund. “In normal times distance by itself does not increase mortality (...) With a well-functioning system, critically ill patients are transported to the ICU even if this is distant,” he explains. But when the system collapses, patients closer to the hospital are prioritized by ambulances because more can be transported in less time.
A total of 14.7 million people in Venezuela have to travel over 6.2 miles (10 kilometers), the distance mentioned in Ciminelli’s analysis, to reach treatment. For half of the country’s population, sentinel centers are far in an emergency.
What happens in Zulia and Sucre—few centers for big populations and rural areas without treatment options—also happens in at least 10 additional states: Falcón, Táchira, Bolívar, Apure, Monagas, Barinas, Lara, Anzoátegui, Mérida and Trujillo. In total, 12 out of all 23 states.
Even as local authorities have designated new sentinel centers, they are not mentioned in official lists or documents. The list with COVID-19 public treatment centers published in March has not been updated in five months.
Methodology
This spatial analysis had a central premise: people will choose the nearest sentinel center (driving distance) to seek COVID-19 treatment.
In order to calculate how far these treatment centers were from the Venezuelan population, we started by geolocating (WSG 84) all COVID-19 treatment centers. Using Google Maps, we searched for 46 sentinel centers and confirmed their location by consulting people familiarized with the particular hospital or CDI. Then, we followed two methodologies:
- Using remote sensing data, we identified 80 cities with over 50,000 people, located their nearest sentinel centers and calculated the driving distance.
- Using 11,432 geocoded communities, we repeated the process, locating the nearest treatment center for each population and measuring the road distance between the center and the community.
In the first case, we used the Global Human Settlement Urban Centre Database 2015, a geographic database by the European Commission’s Joint Research Centre (JRC), which maps world cities. This database uses high resolution satellite imagery, demographic census and other kinds of data to model world urban centers. We used a geographic information system software (ArcGIS) to extract all urban centers within the Venezuelan territory from this database. We found 80 cities. Then we used Google Maps to search for the nearest center for each city and we measured the distance.
In the second case, we loaded four different geographic vector datasets into ArcGIS: one with 46 sentinel centers; one with 11,432 nationwide electoral centers and their voting population; a road network that included 267,484 highways, avenues and streets; and another layer with Venezuela’s territorial subdivision by counties (parroquias), by the United Nations Office for the Coordination of Humanitarian Affairs (OCHA). To start, we overlaid the 11,432 points with the counties dataset, and created a new database where every electoral center was also located by county and municipality. Then we used GIS to perform several network and proximity analysis. To develop the driving-distance (isodistance) map, we did a service area analysis. To get the average distance for each county, we found the nearest sentinel center for each of the 11,432 electoral centers and measured the distances. Then we weighted the results by voting population: first by county, then by state and finally by country. We used electoral centers as a proxy for population density and location. To find total serviced population by each treatment center we matched official 2015 census data by Venezuela’s National Statistics Institute (INE) with our county database, we grouped counties by nearest treatment center and we added the populations. If a county had more than one nearest treatment center, we chose the most important center, the one that served larger populations.
Infographics by: John Fuentes