October 10, 2014 | Pulitzer Center
By
Sascha Garrey
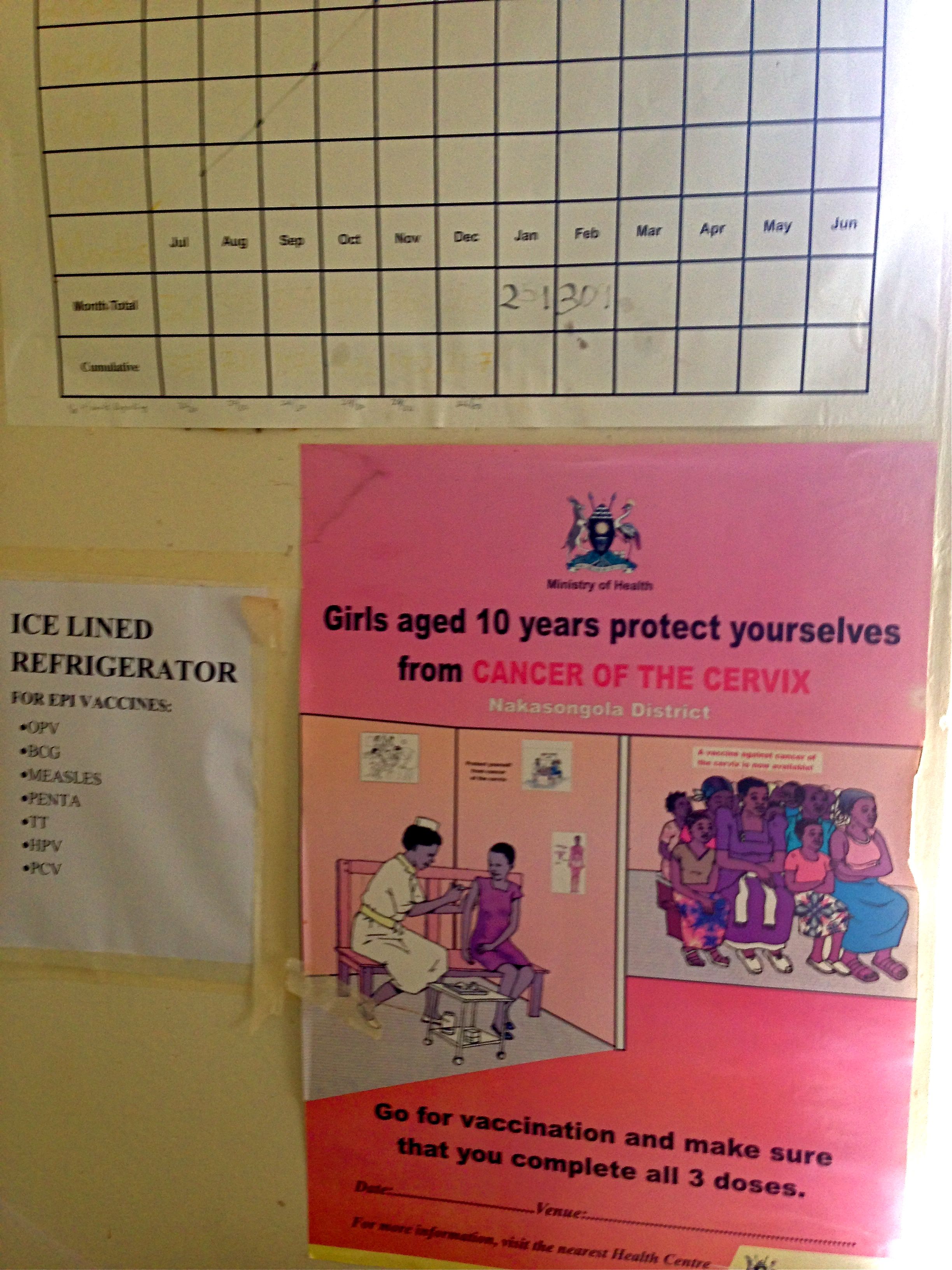
In 2007, a pilot project took place in two districts in Uganda to test different methods of delivering Human Papillomavirus (HPV) vaccines to girls between the ages of 10 and 15. The vaccine used—and that continues to be administered in Uganda—was Gardasil, an immunization owned by Merck that protects against HPV strains 6, 11, 16 and 18, the latter two of which are highly related to the development of cervical cancer.
The Nakasongola District of Central Uganda was one of the trial districts. Although most schoolgirls have been vaccinated consistently since the pilot project, recent financial constraints have posed serious threats to its continued success.